Trauma definition and vulnerable population
American Psychological Association defined trauma as an emotional feeling and response that results from a terrible event like rape, natural disaster, or even accident. It can also be defined as an experience that causes an intense physical and psychological stress reaction in the individual. Trauma normally results from traumatic events, which are those events that put an individual at a closer risk of serious harm or even death. These events can be single or multiple and can include life-threatening experienced that are emotionally harmful and has lasting adverse effects on the individual’s social, physical, and spiritual well-being. Trauma is a normal feeling, and it can happen to anyone, irrespective of age.
The effects of trauma vary with an individual, and there are usually ways of coping with trauma when one is overwhelmed. Trauma has no boundaries and can affect anyone regardless of gender, age, socioeconomic status, race, ethnicity, or sexual orientation. However, adults and children with a history of mental and substance use disorders are more vulnerable to experiencing trauma in their lives (Minot, 2017). Trauma can also be experienced more by elderly people, those living in poverty, marginalized community members, and people with disabilities. In America, about 7-8 people in 100 people suffer from trauma at some point in their lives, with women experiencing more cases of trauma compared to me.
Experience of trauma on an intergenerational level
Trauma leaves lasting damaging effects on an individual and can affect their parenting, communication, and connection with siblings. Intergenerational trauma is the impact that results from a traumatic experience not only to one generation but to other generations. Intergenerational trauma normally results from unawareness of an impact of an event, thus subjecting the next generation to the effects of the traumatic experiences (King-White, 2020). One way trauma can be experienced at the intergenerational level is when a child has been exposed to the trauma of a parent indirectly, resulting in the child experiencing the effects. This cycle can repeat itself, and in some instances, a parent will unintentionally place a child in similar situations that will lead to the child experiencing or suffering from trauma.
Some instances that can play a big role in intergenerational trauma include parental incarceration, where the children and the family members may be affected by the traumatic feeling and emotions that their parent is going through when incarcerated. Divorce or alcohol use disorder, domestic violence, and even child abuse can contribute to intergenerational trauma and may have adverse effects on an individual’s family and the individual’s lifespan. Historical events can also result in intergenerational trauma, more so collective trauma, where a group of people experience the same traumatic event and are impacted similarly. This kind of trauma can last for many generations.
Pathophysiology of Trauma
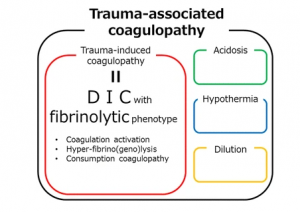
Pathophysiology of trauma refers to the disordered physiological processes resulting from an individual suffering from trauma. Trauma adversely affects body functions, leading to decreased organ perfusion, cellular ischemia, and a cascade of edema and inflammation (Hori & Kim, 2019). Cellular ischemia is caused as a response to mechanical trauma, where the cells lose their integrity and function, thus eventually leading to cellular death. In acute trauma experiences, it results in traumatic coagulopathy, which may cause shock, hypoperfusion, and vascular damage. This coagulopathy consists of coagulation activation, hyperfibrinolysis, and consumption coagulopathy. Early pathophysiology of trauma cab causes an immediate threat to life, with long-term pathophysiology leading to critical care and sepsis in patients. Shock, as one of the pathophysiology of trauma, is the abnormality in the circulation system resulting in inadequate organ perfusion and oxygen delivery. Shock can be classified as hypovolemic, cardiogenic, obstructive, or distributive.
Correlation of Trauma effects with social determinants
Trauma can be considered a social determinant by itself, and in recent studies, a connection between traumatic events and physical health outcomes has been proved. Social determinants are the conditions of the environment that may affect a wide range of health functioning and the quality of life outcomes and risks. Various social determinants increase the risk of an individual’s trauma effects (Sousa, Kemp & El-Zuhairi, 2019). These social determinants include poverty, neighborhood crime and violence, and racism. People living in poverty survive in vulnerable living conditions and have limited access to basic things like food and shelter. The emotional and mental stress in accessing these basics can attract traumatic experiences in these individuals. Also, people living in poverty are prone to life-threatening accidents and physical assaults, which may pre-expose them to traumatic experiences.
Living in neighborhood crimes or violent areas can also increase the likelihood of post-traumatic stress. In a study on this topic, 43% of patients admitted to the Chicago trauma center hospital had trauma signs, with half of those patients being gunshot victims. Racism and, discrimination, social injustice on people can result in racial trauma. This is where Black or Latino Americans suffer from disproportionate treatment that may lead to deaths. This makes Black or Latino Americans suffer from the complex trauma of worrying about what may happen to them. This illustrates how social determinants relate to traumatic effects.
Signs/Symptoms of Trauma
Trauma symptoms vary from mild traumatic effects to severe. Many factors can determine whether an individual is suffering from traumatic effects. The symptoms can be either physical or emotional. Physical symptoms can include shaking or trembling, inability to pay attention, insomnia, tense muscles, hyper-observant, and loss of appetite (Leonard, 2020). Emotional symptoms of trauma include anger, mood swings, violent outbursts, anxiety and fear, panic attacks, guilt, and shame, withdrawing from others, feeling disconnected or feeling numb, and obsessive and compulsive behaviors. An individual can also feel depressed.
Difference between Trauma therapy and trauma-informed care
Trauma-informed care refers to a framework used for human delivery. It is based on knowledge and the understanding of the effects of trauma on people and how it affects their life, service need, and usage. This framework requires changes to an individual’s practices, policies, and culture to create awareness, skills, and knowledge needed for surviving trauma (DeCandia, 2017). On the other hand, trauma therapy refers to the specific approach that recognizes and emphasizes understanding how traumatic effects can affect and impact an individual. Traumatic therapy focuses on an individual’s needs and conditions and helps individuals to deal with their traumatic conditions.
Triggers of trauma-related issues
A trigger can be a stimulus that brings back the memory of a traumatic event or a specific portion of a traumatic experience. A trigger can overwhelm an individual with stress and anxiety by having flashbacks of negative memories about a traumatic event. Triggers can occur in many forms and can be in the form of a physical location that relives a traumatic event about the location or can be an anniversary of a traumatic event that happened in one’s life. Various factors can determine if an individual is suffering or experiencing trauma-related stress (Minot, 2017). These symptoms may include nightmares, flashbacks, severe anxiety, and uncontrollable thoughts about certain events. People suffering from trauma-related stress have difficulties adjusting and coping with circumstances, and they experience reflexes when faced with specific triggers about their traumatic experiences.
Noncompliance or non-adherence to trauma-based behavior history
Patients with a history of trauma can have behaviors that illustrate noncompliance or non-adherence. Noncompliance is when the patient suffering from trauma deliberately refuses to follow the treatment plan of therapy aimed at helping the patient recover from the traumatic effects. Non-adherence, on the other, is where a patient suffering from traumatic stress unintentionally fails to follow the treatment plan designed to help the patient recover. Various behaviors could make a person with a trauma history be regarded as non-compliant or non-adherence (Haller et al., 2022). One of the behaviors is fear. Patients with traumatic stress are sometimes frightened by the side effects of the treatment and medicine, which may make the patients stop taking the treatments intentionally due to the fear of suffering side effects.
Cost may also make a patient stop following a traumatic stress treatment unintentionally because the patient may be unable to cater for the treatment due to the high cost of the medicine or therapy, which may be interpreted as non-adherence. Too many medications may make a patient from following a traumatic stress treatment. Medications with higher dosing frequency may increase the chances of a patient forgetting to take the medications, which may be termed non-adherence. Worry is another factor that can be taken as a behavior for noncompliance or adherence. This is because if a patient suffering from trauma becomes worried about becoming dependent on the treatment medicine, it can lead to non-adherence.
Trauma and Substance Abuse
Decades of research have identified a strong link between exposure to traumatic events and substance use disorder. In a study, SAMHSA found that among patients suffering from substance use disorder, 20.3 million aged 12 and above had a traumatic experience at least once in their lives (Abuse, 2019). Therefore, individuals with substance use disorder are more likely to experience traumatic events. The connection between the two is very wide, with different types of SUD having a close connection with trauma. Substance use is taken by people suffering from traumatic effects as one way to counter traumatic emotions. More so, there is a high risk that people who use substances live in areas where they have experienced traumatic events, and their lifestyles, therefore, match those of substance use.
Individuals who use substances are also very likely or susceptible to developing post-traumatic stress disorder after exposure to trauma than those who do not use substances. One-quarter to three-quarters of people who survive abusive and traumatic experiences usually report having a problem with alcoholism. Most veterans who experienced post-traumatic abuse have all met the criteria for being diagnosed with PTSD. Individuals who suffer from substance use disorder usually experience traumatic reflexes in their lives, with women showing increased alcohol use disorder when exposed to traumatic events.
Conclusion
Traumatic experiences occur as s a result of traumatic events that an individual undergoes or had undergone in life that left him or her physically, mentally, and spiritually emotionalized. Trauma destabilizes the emotional, psychological, and physical aspects. Trauma makes an individual lose hope in life due to the negative feelings that sometimes overwhelm them. Trauma can result from events like accidents, disasters, and trauma experiences differ from person to person, with coping Factors also varying between individuals. Substance use has a very close relationship with trauma, with many individuals with trauma resorting to substance use to cope with the negative feeling.
References
Abuse, S. (2019). Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration.
DeCandia, J. C. 2017. Trauma-Informed Care and Trauma-Specific Services: A Comprehensive Approach to Trauma Intervention. American Institutes for Research (AIR) (Washington DC)
Hori, H., & Kim, Y. (2019). Inflammation and post‐traumatic stress disorder. Psychiatry and Clinical Neurosciences, 73(4), 143–153.
Sousa, C. A., Kemp, S. P., & El-Zuhairi, M. (2019). Place as a social determinant of health: Narratives of trauma and homeland among Palestinian women. The British Journal of Social Work, 49(4), 963-982.
Leonard, J. (2020, June 3). What is trauma? Types, symptoms, and treatments. Www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/trauma
King-White, D. (2020, July 31). Intergenerational Trauma: What It Is & How to Heal. Choosing Therapy. https://www.choosingtherapy.com/intergenerational-trauma/
Minot, D. (2017, July 1). Why Trauma-Informed Care with Vulnerable Populations? Behavioral Health News. https://www.behavioralhealthnews.org/why-trauma-informed-care-with- vulnerable-populations
Haller, K., Fritzsche, S., Kruse, I., O’Malley, G., Ehrenthal, J. C., & Stamm, T. (2022). Associations Between Personality Functioning, Childhood Trauma and Non-adherence in Cardiovascular Disease: A Psychodynamically-Informed Cross-Sectional Study. Frontiers in Psychology, 13.